Burn injuries present a significant challenge in medical care, demanding precise diagnosis and meticulous management to optimize outcomes. The critical aspects of diagnosing and treating burns, from initial severity assessment to long-term care considerations, can greatly impact a patient’s long-term prognosis. The various methodologies employed by clinicians to ascertain burn depth and extent, such as the Rule of Nines and the Lund and Browder chart, can shape therapeutic approaches and prognoses. Additionally, specific conditions like inhalation injuries can provide additional diagnostic and treatment complications that must be managed effectively. Doing so ensures a holistic approach to burn recovery that supports both physical healing and psychological rehabilitation.
Diagnosing Burn Severity
Diagnosing burn severity is a critical step in the management and treatment of burn injuries. Clinicians utilize various methodologies to ascertain the degree and depth of burns, which directly influence the therapeutic approach and prognosis. Each method provides vital information that contributes to a comprehensive understanding of the injury’s impact. Accurately evaluating burn severity requires a combination of visual assessments, physical examinations, and specialized tools such as the Rule of Nines and the Lund and Browder chart. These assessments ensure patients receive precise and tailored treatment, enhancing recovery outcomes and minimizing potential complications.
Clinical Assessment of Burns
Assessing the severity of burns is critical for determining appropriate treatment and predicting recovery outcomes. Initially, clinicians evaluate the burn’s depth, which significantly impacts therapeutic decisions. Superficial burns often heal with minimal intervention, whereas deeper burns may necessitate surgical procedures such as skin grafting.
Furthermore, the extent of the burn is quantified using the “rule of nines” or Lund and Browder chart, tools that help estimate the total body surface area (TBSA) affected. This measurement is crucial, especially when considering fluid resuscitation protocols and potential complications.
Depth Assessment:
- First-degree burns affect only the epidermis and usually present with redness and pain.
- Second-degree burns can be more severe, impacting the dermis, and often feature blisters and intense pain.
- Third-degree burns extend through the dermis, destroying the affected skin, which becomes white, leathery, or charred.
Extent Evaluation:
- Using the “rule of nines,” an adult’s entire arm represents approximately 9% of the body surface area, facilitating quick assessment in emergency situations.
- The Lund and Browder chart adjusts for age, providing more accuracy with children.
In addition to depth and extent, the burn’s location is also considered. Burns on the face, hands, feet, and over major joints are particularly concerning due to the potential for functional and cosmetic impairment.
Moreover, the patient’s overall health and pre-existing conditions influence the management plan. Those with cardiovascular diseases or diabetes may face slower recovery and higher complication rates.
Finally, checking for inhalation injury is essential, a common and serious complication in patients exposed to fires. Symptoms such as wheezing, coughing, or difficulty breathing require immediate attention to secure the airway and support respiratory function.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
Classification of Burns
Classification of burns is essential for clinicians to determine appropriate care and treatment. Burns are primarily categorized into three degrees, each indicating a different level of severity and skin damage.
- First-Degree Burns: These are the mildest form of skin injuries. First-degree burns are not serious; they only affect the outer layer of the skin, known as the epidermis. Characteristics include redness, slight swelling, and pain. Typically, they do not form blisters and usually heal within a week without long-term scarring.
- Second-Degree Burns: More severe than first-degree, these burns damage both the epidermis and the dermis. They present with swelling and redness, accompanied by blistering. The skin may appear shiny and feel very tender. Depending on the depth of damage, they can be classified further into superficial and deep partial-thickness burns. Superficial ones generally heal in two to three weeks, whereas deep partial-thickness burns might require more than three weeks and could lead to some scarring.
- Third-Degree Burns: Third-degree burns are the most serious type. Third-degree burns destroy the full thickness of the skin, extending into the subcutaneous layers. The affected area can appear white, charred, or leathery. These burns typically do not exhibit pain immediately, as the nerve endings are destroyed. Healing from third-degree burns usually requires surgical intervention, such as skin grafting, due to the extensive damage.
Moreover, the severity of the burn influences the potential for complications. For instance, third-degree burns can lead to significant fluid loss, infection, and changes in the body’s temperature regulation. Each degree of burn requires specific medical interventions, from pain management and topical creams for first-degree burns to more complex surgical needs for third-degree burns.
Assessing Burn Depth
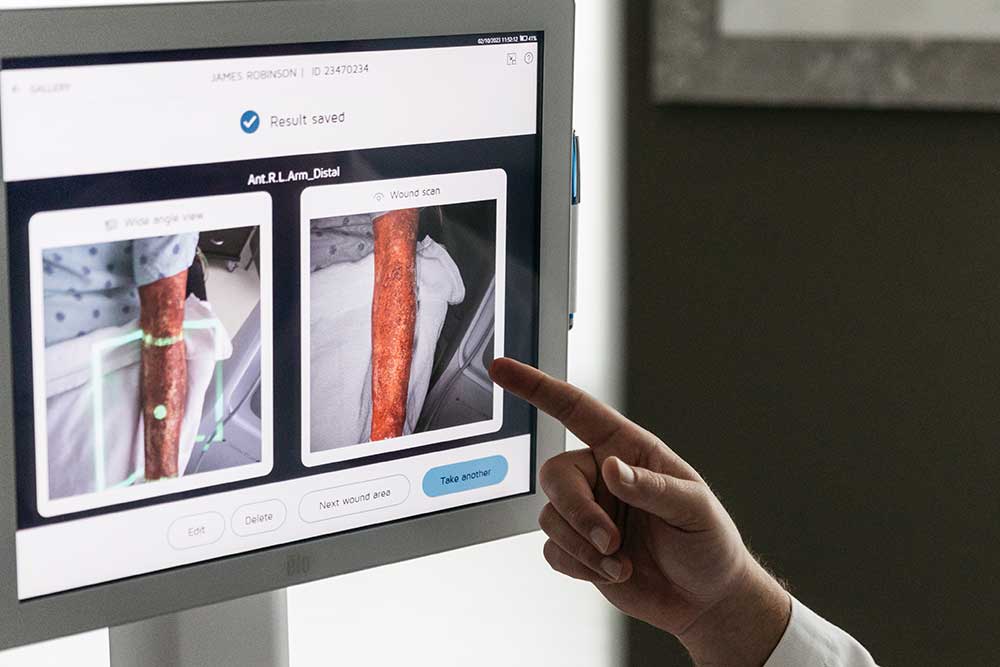
Assessing the depth of burn injuries is crucial for clinicians to effectively manage and treat patients. Accurate assessment aids in determining the severity of the burn, which influences treatment decisions and predicts potential complications. There are several methods available to evaluate burn depth, including visual assessment, physical examination, and diagnostic tools like the Rule of Nines and the Lund and Browder chart.
Visual assessment involves examining the appearance of the burn. Clinicians look for cues such as color, texture, and the presence of blisters. Generally, a redder appearance indicates superficial burns, while a white or charred look suggests deeper damage.
Physical examination includes testing the sensitivity of the area to touch. Burns with intact sensation typically involve less depth, whereas those with no sensation may extend deeper into the skin layers.
- Rule of Nines: This method is used primarily in adult patients to estimate the total body surface area (TBSA) affected by burns. The body is divided into sections, each accounting for approximately 9% (or multiples thereof) of the total body area. It provides a rapid assessment tool in emergency settings.
- Lund and Browder Chart: Offering more precision than the Rule of Nines, this chart is especially useful for children, as it accounts for the proportional differences in body surface area with age. It provides detailed sections and modifies percentages based on the patient’s development stage.
Additionally, clinicians may employ diagnostic imaging, such as ultrasound or laser Doppler, to assess burn depth more accurately when the visual and physical examinations yield inconclusive results.
Treatment Strategies for First-Degree Burns
Immediate Care for Skin
Immediate care for first-degree burns is crucial in reducing pain, preventing complications, and facilitating healing. Proper first aid not only alleviates discomfort but also minimizes tissue damage and promotes quicker recovery. The primary goals in treating first-degree burns involve cooling the burn promptly, protecting the injured skin, and managing pain.
Upon assessing a first-degree burn, the initial step should always be to cool the affected area. This action helps to halt the burning process, reduce swelling, and lessen pain. Clinicians recommend gently running cool (not cold) water over the burn for several minutes. It is essential to avoid ice or excessively cold water, as these can cause further tissue damage.
After cooling, the burn should be covered with a clean, dry cloth or a sterile non-adhesive bandage. This covering serves multiple purposes:
- Protects the burn from contamination, reducing the risk of infection.
- Shields the sensitive area from further physical irritants.
- Helps maintain moisture at the site, which is beneficial for the healing process.
In addition to these immediate actions, clinicians advise against the use of butter, oils, or any home remedies, which can exacerbate the injury. Over-the-counter pain relievers like acetaminophen or ibuprofen can be effective for managing discomfort associated with first-degree burns.
Moreover, monitoring the burn for signs of infection, such as increased redness, swelling, or pus, is vital. If any of these symptoms occur, further medical evaluation may be necessary.
Wound Management for Burns
Effective wound management for first-degree burns is fundamental in preventing infection and promoting optimal healing. Clinicians focus on several key techniques including gentle cleaning, application of suitable dressings, and regular monitoring to ensure the wound heals properly.
Firstly, it is essential to clean the burn area gently with mild soap and water to remove any debris and contaminants. This simple step helps to prevent infection, a common complication that can significantly delay healing. After cleaning, the burn should be dried carefully to avoid irritation.
Subsequently, clinicians apply a thin layer of aloe vera or an antibacterial ointment, which serves to soothe the burn and reduce the risk of infection. Choosing the right dressing is crucial; for first-degree burns, a non-adhesive, sterile gauze pad is often recommended. This type of dressing absorbs any fluid discharge, maintains a moist environment conducive to healing, and allows the skin to breathe.
Regular dressing changes are imperative to assess the wound’s progress and maintain cleanliness. Typically, dressings should be changed once daily, or more frequently if they become wet or soiled. Each change provides an opportunity to inspect the burn for signs of infection, such as increased redness, swelling, or oozing, which would necessitate a reassessment of the treatment approach.
Additionally, ensuring patient comfort during dressing changes is vital. Gentle handling and explaining each step can alleviate anxiety and pain associated with the process. Pain management may include over-the-counter medications like acetaminophen or ibuprofen, particularly if the burn is causing significant discomfort.
Pain Management for Burns
Effective pain management is a critical component of the treatment strategy for first-degree burns. Addressing pain not only improves patient comfort but also facilitates better overall healing outcomes. For first-degree burns, which typically involve minimal tissue damage, a variety of non-pharmacological and pharmacological methods can be employed to manage discomfort.
Initially, clinicians recommend cooling the burn immediately after injury by gently running lukewarm water over the area for several minutes. This simple yet effective method helps reduce the skin temperature, alleviate pain, and limit damage to the surrounding tissues.
Following the initial cooling, appropriate wound care is vital. Applying aloe vera gel or a hypoallergenic moisturizer can soothe the burn and provide a protective barrier that aids in reducing irritation. Over-the-counter topical lidocaine, an anesthetic, can be used to numb the area, offering additional pain relief.
For persistent pain, oral pain relievers such as acetaminophen or ibuprofen are advised. These medications help manage inflammation and discomfort, making it easier for patients to engage in normal activities while healing.
Clinicians also emphasize the importance of regular dressing changes to prevent infection and manage pain. Using non-adhesive, sterile gauze pads protects the burn and minimizes pain during dressing changes. Ensuring the burn area is kept clean and dry under the dressing helps prevent additional irritation and discomfort.
Lastly, monitoring for signs of increased pain or infection is crucial, as these could indicate complications requiring more intensive treatment. By implementing these pain management strategies effectively, clinicians can significantly enhance the quality of care for patients with first-degree burns, promoting faster recovery and minimizing distress.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
Special Considerations for Burn Victims
When treating burn victims, clinicians face numerous challenges that extend beyond initial wound care. Special considerations such as inhalation injuries, potential complications, and long-term care strategies are paramount to ensure comprehensive treatment and rehabilitation. Inhalation injuries, for example, require urgent and precise management to prevent respiratory complications, a common and serious threat in burn care. Meanwhile, clinicians must vigilantly prevent and manage other complications like infections and fluid imbalances, which can severely impact recovery if not properly addressed. Moreover, the path to recovery continues well beyond the acute phase, as long-term care involves a multidisciplinary approach to help patients regain functionality and quality of life. This section delves into these critical aspects, highlighting the intricate and dedicated efforts required to support burn victims throughout their healing journey.
Inhalation Injuries
Inhalation injuries in burn victims can significantly impact recovery and require immediate attention. Inhalation injuries often accompany facial and upper torso burns, necessitating a comprehensive approach to assessment and treatment.
Firstly, clinicians must quickly assess the airway for any signs of obstruction or damage. Signs such as soot around the nostrils or in the mouth, singed nasal hair, hoarseness, and difficulty breathing indicate the need for urgent evaluation. In such cases, securing the airway takes precedence to prevent respiratory distress.
Following stabilization, bronchoscopy is often employed to evaluate the extent of the respiratory tract damage. This diagnostic tool allows for a direct visual assessment of the airways, helping to identify the presence of soot, edema, and mucosal damage.
Treatment strategies then focus on maintaining airway patency and managing complications. Humidified oxygen is frequently administered to support breathing and reduce the risk of hypoxia. In cases of significant swelling or obstruction, intubation may be necessary to ensure that the patient can breathe adequately during recovery.
Moreover, proper wound care for associated burns is critical. Regular debridement and dressing changes help prevent infection and promote healing of the skin and tissues damaged by the fire. Dressings should be changed under sterile conditions to minimize the risk of introducing pathogens into the wound.
Clinicians also monitor for pulmonary complications such as pneumonia, which are common in patients with inhalation injuries. Prophylactic antibiotics may be administered as a preventative measure, depending on the severity of the inhalation injury and the clinical judgment of the treating physician.
Complications
Infection stands as one of the most common and severe complications in burn care. The loss of skin integrity exposes the body to microbial invasion, making meticulous wound care and aseptic techniques paramount. Regular cleaning, debridement, and sterile dressing changes are critical to prevent bacterial and fungal infections.
Moreover, fluid imbalance is a significant concern immediately after a burn due to increased capillary permeability and fluid loss through the injured skin. Clinicians must manage fluid resuscitation carefully to maintain adequate circulation and prevent both dehydration and fluid overload, which can lead to pulmonary edema.
Another complication is the development of hypertrophic scars and contractures, particularly with deeper burns. These can impair mobility and functionality, requiring early intervention with physical therapy and possibly surgical procedures to release contractures.
Systemic responses such as the hypermetabolic state triggered by severe burns also require special attention. This condition increases caloric needs dramatically; therefore, nutritional support through high-protein and high-calorie diets becomes essential to support wound healing and overall recovery.
Lastly, clinicians monitor for respiratory complications, especially in cases of inhalation injury. Pulmonary function may be compromised, necessitating respiratory support and careful monitoring for signs of acute respiratory distress syndrome (ARDS).
Long-Term Care
Effective long-term management typically involves a multidisciplinary team approach. This team coordinates various treatments and support mechanisms tailored to the individual needs of each patient. Key components include physical therapy to restore mobility and strength, and occupational therapy to help victims return to daily activities and work.
Regular follow-up appointments are crucial for monitoring the healing of burns, assessing the development of scar tissue, and implementing interventions like scar management therapies. Options such as silicone gel sheets, pressure garments, and possibly non-invasive laser treatments can significantly improve the appearance of scars and the elasticity of the skin.
Psychological support also plays a vital role in the long-term care of burn victims. Counseling and support groups can aid in addressing the emotional trauma associated with disfiguring injuries, helping patients to cope with body image changes and reintegrate into social environments.
Nutritional guidance is another critical aspect, as proper nutrition supports wound healing and overall health. Dietitians may recommend high-protein, high-calorie diets to meet the increased metabolic demands following severe burns.
Furthermore, clinicians often collaborate with social workers to provide resources and support for vocational rehabilitation and community reintegration, ensuring patients receive the necessary assistance to navigate their recovery journey effectively.
In conclusion, diagnosing and managing burn severity is a complex yet critical aspect of medical care, requiring detailed assessments and a multidisciplinary approach. Clinicians rely on accurate evaluations of burn depth and extent using tools like the Rule of Nines and the Lund and Browder chart to tailor treatment plans effectively. The proper classification and ongoing assessment of burns, from superficial to full-thickness injuries, ensure that each patient receives the specific interventions needed to optimize healing and minimize complications. Furthermore, addressing potential challenges such as inhalation injuries and complications like infection or fluid imbalance early in the treatment process is vital for improving outcomes. Ultimately, the diligent application of these diagnostic and management strategies enables healthcare providers to offer the best possible care to burn victims, supporting their recovery from initial injury through to long-term rehabilitation.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?