A wound imaging device is an essential tool in modern wound care, particularly for clinicians managing burns and traumatic injuries. These devices use advanced technologies like high-resolution cameras, thermal and infrared imaging, and 3D surface mapping to provide detailed and accurate assessments of wound depth, surface area, and tissue health. By offering real-time insights, wound imaging devices allow clinicians to make informed decisions about treatment, track healing progression, and detect complications early. The integration of artificial intelligence and portable designs has further enhanced their functionality, making them indispensable in both emergency rooms and long-term wound care management.
What is an Imaging Device for Wounds?
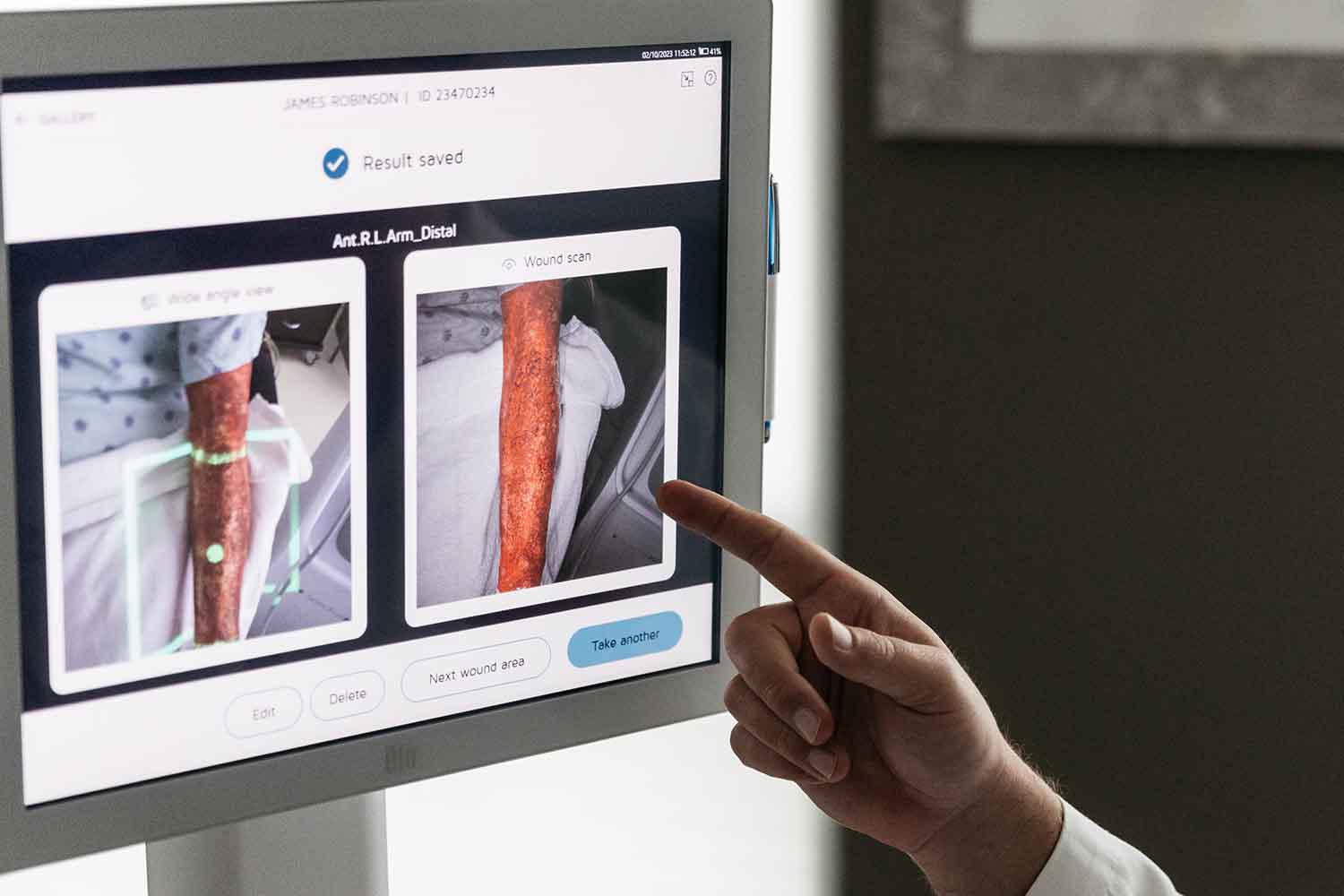
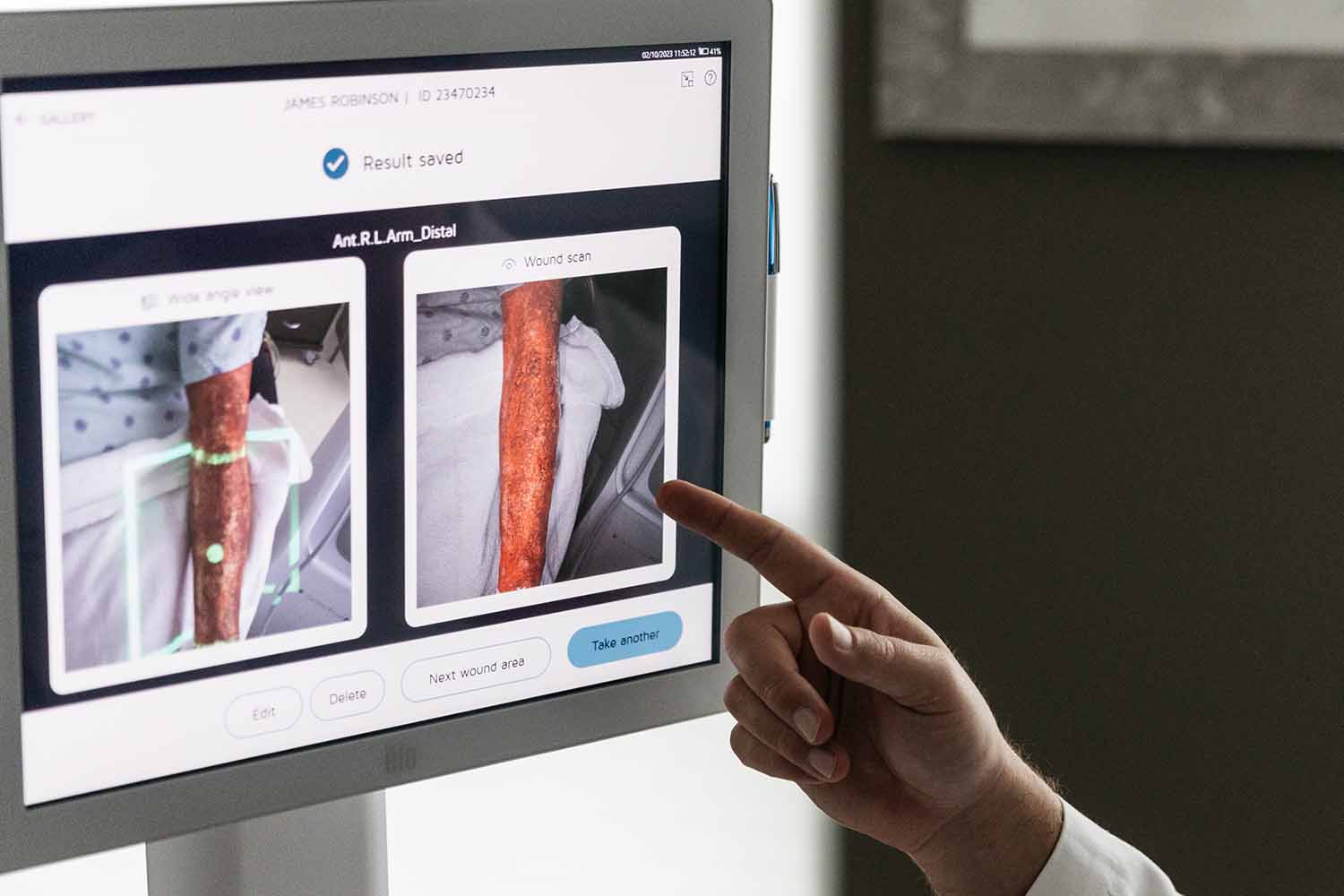
A wound imaging device can be a valuable tool in assessing wounds as it captures detailed visual information to assess the extent, depth, and severity of various injuries, including burns, lacerations, and ulcers. These devices provide clinicians with high-resolution images, helping them to evaluate tissue damage, monitor healing progress, and identify complications such as infections.
Key features of wound imaging devices include:
- High-resolution cameras: These capture minute details in color and texture, allowing for precise visualisation of the wound area.
- Infrared and thermal imaging: Infrared technology helps detect blood flow, while thermal imaging highlights inflammation or infection, offering deeper insights into the wound’s condition beyond what the naked eye can perceive.
- 3D imaging capabilities: Some devices generate three-dimensional representations, giving clinicians a full perspective on wound topography, enabling more accurate measurements of size and depth.
- Automated wound measurement: Built-in software analyses wound size, surface area, and changes over time, reducing the need for manual calculations and improving accuracy.
Wound imaging devices are highly valuable in emergency and burns care settings. They facilitate the documentation of injury progression, guide treatment decisions, and provide objective data for patient records. These tools also aid in wound debridement, surgical planning, and determining when advanced therapies like skin grafts may be necessary.
Transitioning from traditional wound assessments to imaging devices enhances diagnostic precision, making wound management more efficient. By offering real-time feedback, these devices help clinicians make timely and informed decisions, ensuring patients receive optimal care.
The Importance of Wound Imaging
Wound imaging technology has become essential for enhancing wound care and improving patient outcomes, particularly in burn treatment and emergency settings. It provides clinicians with the ability to assess wounds in a more detailed and objective manner, overcoming limitations of traditional visual inspections. By offering advanced features such as automated measurements and thermal imaging, wound imaging devices elevate both the precision and efficiency of wound care.
Key advantages of wound imaging include:
- Refined wound assessment: Wound imaging allows for more detailed visualisation of injuries. This includes assessing wound depth, surface area, and identifying tissue necrosis or viable tissue. In burns care, this detailed assessment helps determine the severity and need for surgical interventions or specialised treatments.
- Objective data collection: Traditional wound measurement methods, such as rulers or manual tracing, can be subjective and prone to variation. Imaging devices provide consistent, quantifiable data, allowing for standardised wound measurement across different care providers and facilities.
- Enhanced healing monitoring: By documenting the progression of wound healing, imaging offers a clear view of tissue regeneration or complications. This allows clinicians to adjust treatment protocols as necessary, such as determining when a wound is healing adequately or when additional therapies like grafting may be needed.
- Complication detection: Early recognition of wound complications, such as infection or poor perfusion, is critical in wound management. Advanced imaging modalities, including thermal imaging, help detect these issues early, often before they become clinically visible, thus allowing for prompt intervention.
By improving wound assessment accuracy and providing real-time feedback, imaging devices lead to more informed clinical decisions. This technology ultimately enhances wound management practices, resulting in more effective treatments and improved recovery for patients.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
The Technology
Advanced Imaging Techniques
Advanced imaging techniques have dramatically improved the way clinicians assess and treat wounds, particularly in the context of burns and acute trauma. By offering more detailed and precise information, modern imaging tools help clinicians evaluate wound characteristics that go beyond what is visible to the naked eye. This precision reduces uncertainties in diagnosis and ensures tailored treatment plans for each patient.
Common imaging modalities in wound care include:
- High-resolution photography: Using specialised cameras, clinicians can capture detailed images that reveal subtle variations in skin texture, color, and wound edges, which aids in tracking changes over time.
- Thermal imaging: This tool detects heat patterns in the skin, revealing inflammation, compromised blood flow, or potential infections. Its non-invasive nature makes it ideal for frequent monitoring, allowing clinicians to identify problems early.
- Infrared spectroscopy: By analysing tissue oxygenation and perfusion, infrared imaging provides critical data on whether a wound is healing appropriately or requires more aggressive interventions to promote tissue recovery.
- 3D surface imaging: This technique generates three-dimensional representations of the wound, enabling clinicians to assess wound depth and topography with unparalleled accuracy.
The benefits of these advanced imaging techniques include:
- More precise surgical planning: 3D imaging helps surgeons visualise wounds more clearly, allowing them to approach debridement and grafting with greater accuracy.
- Early complication detection: Technologies like thermal and infrared imaging can identify problems such as infection or necrosis before they are clinically visible, enabling early intervention.
By incorporating advanced imaging into wound care, clinicians gain a comprehensive understanding of injury dynamics, ultimately leading to faster healing and better patient outcomes.
Innovations in Imaging Devices
By incorporating new technologies, wound assessment has become not only more efficient but also more predictive, enhancing patient outcomes.
Some of the most significant advancements include:
- Miniaturisation and portability: New portable imaging devices are now small enough to be easily used in emergency settings or at the patient’s bedside. This allows for quick, high-quality assessments without the need to transport patients to specialised imaging centres.
- AI and machine learning integration: The use of artificial intelligence in wound imaging is revolutionising the way clinicians analyse wounds. These systems can automatically identify wound characteristics, measure dimensions, and even predict healing trajectories, reducing human error and improving decision-making accuracy.
- Fluorescence imaging for bacterial detection: Recent innovations in fluorescence technology allow clinicians to visualise bacterial presence directly in the wound. This method is non-invasive and provides immediate feedback on infection risks, facilitating faster and more targeted interventions.
Looking to the future, several emerging trends are poised to further impact wound care:
- Continuous monitoring systems: Wearable wound sensors are being developed to provide ongoing data on wound healing, giving clinicians real-time insights into the wound environment and alerting them to potential issues before they escalate.
- Remote care advancements: With the integration of telemedicine, clinicians can now remotely assess and monitor wounds, ensuring specialised care is available even in resource-limited settings.
The evolution of the wound imaging device has transformed wound care, offering clinicians the ability to assess, diagnose, and treat wounds with unprecedented accuracy. From high-resolution cameras and 3D imaging to AI-powered analytics and fluorescence technology, these devices enable more precise measurement and monitoring of wounds, enhancing treatment outcomes. As advancements continue, emerging trends such as wearable sensors and telemedicine integration will further streamline wound care, ensuring that clinicians can deliver efficient, personalised care to patients even in remote or resource-limited settings. The continued innovation in wound imaging devices promises a future where wound management is more proactive, data-driven, and effective.